Healthcare Professionals Hub
Blood tests
Common blood tests and how to interpret them
Initial investigation of rheumatic symptoms
Rheumatology can be referred to as the ‘Jigsaw Speciality’ as diagnosis is often made by a combination of patient’s symptoms over time, their clinical signs and the results of investigations. Blood tests are key and help both triage and assess referrals.
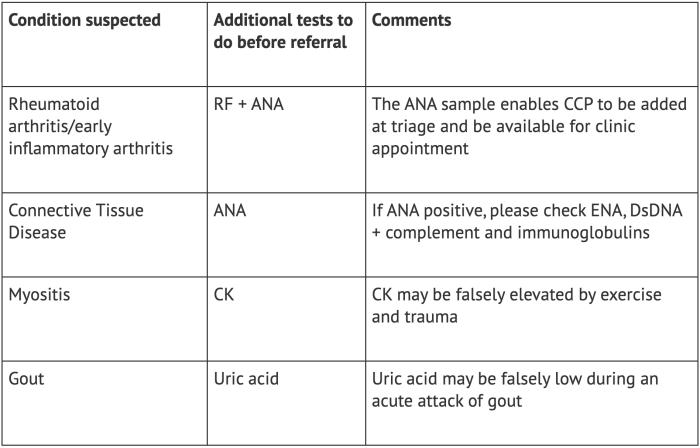
All patients referred to Rheumatology should have a basic set of investigations including CRP, U+E, LFT and FBC, with additional tests depending on condition suspected.
CRP
C-reactive protein (CRP) is sensitive to change and much more specific than ESR in assessing inflammatory symptoms. CRP is likely to be falsely elevated if patients BMI >35 (visceral adipose tissue is metabolically active and produces inflammatory cytokines) and in infection, both of which should be taken into account when interpreting the results. CRP is the investigation of choice for initial diagnosis and subsequent monitoring of patients with PMR and Temporal Arteritis, and when early inflammatory arthritis is suspected.
CRP may be normal in early inflammatory disease – patients with definite visible joint swelling should still be referred for investigation if CRP normal, but referral for possible inflammatory joint disease is unlikely to be useful if no joint swelling and normal CRP.
RF
Rheumatoid factor (RF) is only a useful investigation if you suspect Rheumatoid Arthritis (RA – typically symmetrical small joint pain and swelling). RF is falsely positive in around 5-10% of the normal population, usually at low levels – between 13 and 40. If the patient does not have inflammatory joint symptoms, a Rheumatoid factor of this level does not require referral. RF may be positive at high levels in patients with Hepatitis, and in other Rheumatic diseases such as Sjogrens and SLE.
CCP
Anti-CCP Antibody (CCP) is extremely specific for RA but cannot currently be requested in primary care. We can add a CCP to your patient’s bloods if you request RF and anti nuclear antibody (ANA) prior to referral in patients whom you suspect Rheumatoid Arthritis.
CCP also gives very important information about prognosis, and therefore affects treatment decisions – patients positive for CCP should therefore be assessed by Rheumatology.
ANA
ANA is an initial screening investigation for connective tissue diseases (SLE, Myositis, Scleroderma, Sjogrens), and largely reassuring with regards to these conditions if negative. It is very frequently false positive at low titres. If ANA is positive, additional immunology tests should be checked, including Immunoglobulins, ENA and dsDNA, which are much less frequently false positive, and have clear disease associations if positive. Patients with symptoms of connective tissue disease – joint pain, rash, Raynauds, oral ulcers, dry eyes and mouth, hair loss, fatigue etc and positive ANA/ENA/DsDNa should be referred, and are likely to be triaged to the connective tissue disease clinic.
Uric Acid
Uric acid is helpful in patients suspected as having gout, and is most useful if checked at a time when the patient doesn’t have an acute attack. Uric acid is suppressed during acute attacks of gout due to it leaving the blood and precipitation as crystals in the affected joint(s). When used to monitor the progress of urate lowering treatment, the target for uric acid suppression is usually <300umol/l. There is currently no evidence that patients who have high levels of urate, but who do not have symptoms of gout (acute intermittent joint swelling, usually affecting feet) should receive urate lowering treatment, but should receive lifestyle advice, including reduction in alcohol (particularly beer) and sugary drink consumption.