Healthcare Professionals Hub
Plantar fasciitis
Pathway
Patient presents to GP with heel pain
Clinical diagnosis
To be given a diagnosis of mechanical Plantar Fasciitis (MPF), and enter the Mechanical Plantar Fasciitis pathway, a patient must firstly have no other symptoms suggestive of an underlying systemic cause; then have at least three of the following symptoms:
- Medial tubercle tender
- Plantar fascia tender
- Plantar fascia tender under tension
Pain on 1st Weightbearing, and after a long period of sitting, and at the beginning of weight-bearing activities such as walking
Diagnostic tests (options)
- X-RAY-If non-mechanical cause of PF possible (not to be requested to confirm spurs!!)
- Ultrasound-to confirm PF diagnosis (not standard) or if other causes indicated e.g bursitis, soft tissue lesion, or partial/full tear.
- Bloods-e.g inflammatory conditions
Outcome Measures
Measuring the severity of MPF is difficult; currently there is no specific tool to measure heel pain. However, by using a series of VAS for symptoms or aspects specific to MPF an accurate measure of its severity and progress can be obtained.
Clinical Examinations
- Palpate the medial tubercle. Is it tender?
Have the patient grade the level of tenderness between 0-10 (0 being no tenderness and 10 being the most tenderness they could ever experience - Palpate the plantar fascia. Is it tender?
Palpate the plantar fasica under tension. Is it tender?
Have the patient grade the level of tenderness between 0-10 (0 being no tenderness and 10 being the most tenderness they could ever experience - Palpate the plantar fasica under tension. Is it tender?
Have the patient grade the level of tenderness between 0-10 (0 being no tenderness and 10 being the most tenderness they could ever experience) - The most commonly stated complaints are pain upon first rising, after a long period of sitting, and at the beginning of weight-bearing activities such as walking.
Have the patient grade the level of pain between 0-10 (0 being no pain and 10 being the most pain they could ever experience) - The most commonly stated complaints are pain upon first rising, after a long period of sitting, and at the beginning of weight-bearing activities such as walking
Have the patient mark the number of minutes it takes for these symptoms to ease.0-10 minutes (0 being no minutes and 10 minutes. If it is longer than 10 minutes mark the 10 with an *
Clinical information to document
Occupations: Document extended periods of weight bearing and work shifts of 8 hours and over
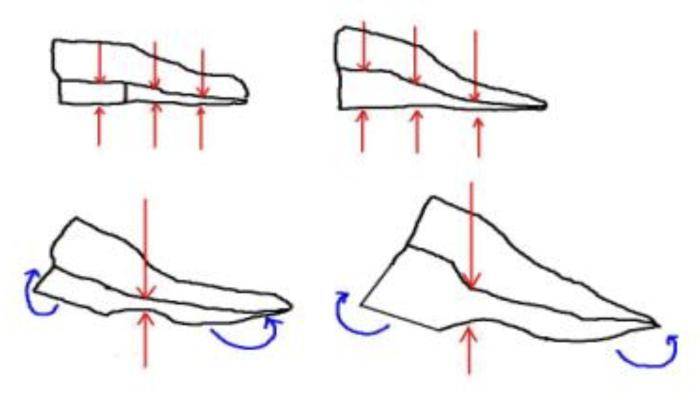
- Document if the patient has excessive foot pronation at the subtalar joint.
- Ankle Equinus: Does the patient have limited ankle dorsiflexion i.e. less than 10 degrees
- Ankle Equinus: Document ankle dorsiflexion in both extended and flexed knee positions to determine if the restriction is due to Gastrocnemius or Soleus tightness, or ankle bony blockade.
- Obesity: Document if the patient is overweight
Footwear test
- A shoe will be defined as having a Heel Counter Defect if it looks like picture B
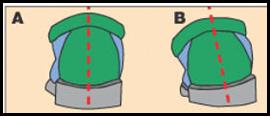
- The sole and heel section of each shoe should be assessed for manufacture defects and excessive wear.
- A compression Test should be performed to determine if the sagittal plane collapse. Press down on the shoe, just anterior to the heel
- Press down on the shoe, just anterior to the heel
Mechanical Plantar Fasciitis – 1st Line Intervention
- The first line intervention should focus on educating the patient about the condition, and prescribing therapies that can be self-administered by the patient
- Activity Modification: For those patients who stand for more than 8 hours per day, reduced activity levels and modified work shifts i.e. less than 8 hours should be advised
- Stretching: Both specific plantar fascial and Achilles tendon stretches should be used.
Specific Plantar Fascial Stretch:
– 10 repetitions x 10 seconds, 3 times daily as per the Giovanni method.
Achilles tendon Stretch:
Either of the following regimes should be used:
– 3mins x 3 times daily 5 sets of 20 seconds, 2 times daily
– Stretch & hold for 10 seconds, relax, and then stretch for another 20 seconds; this should be repeated 20 times
Stretches should be demonstrated to the patient, and then the patient should repeat them back. In addition handouts, with both written and diagrammatic information should be given
Clinical standard: It should be documented that the patient has been shown, understands and agrees to do the stretches. - Footwear Advice: When selecting footwear the patient should be advised not to wear shoes with the following features:
– Compresses/collapses too much in the sagittal plane
– Unstable heel
– Non-supportive (flimsy) heel counter.
– Thin soled shoes
– Badly worn and distorted shoes (ill-fitting) - Low-Dye taping should be used; any of the variations described in the literature can be utilised.
Taping should be kept on a maximum of three days at a time.
Patients can self apply the taping, but must be shown how and given an advice sheet on how to do so. - If NSAID’s have not been tried, then the patient can be advised to consult their GP for a prescription or to consult a Pharmacist for use of over the counter NSAID’s.
If there is an active inflammatory process then use of Ice can be given. - First line Intervention should be given 6-12 weeks, if the patient has not responded by then the clinician can proceed to the Second Line Intervention.
Mechanical Plantar Fasciitis – 2nd Line Intervention
Orthotics:
- The orthotic prescription should be left to the clinician, who should describe the prescription in detail in the patient records.
- The second line intervention should last between 12-24 weeks allowing time for prescription variations to be tried. If the patient has not responded by then the clinician can proceed to the Third Line Intervention
Mechanical Plantar Fasciitis-3rd Line Intervention
Night Splints:
8. A night splint, which applies dorsiflexion to the ankle and the MTPJs should be dispensed.
Night splints should be used for a duration of 12-16 weeks before moving on to the 4th Line Intervention
Mechanical Plantar Fasciitis 4th Line Intervention
Steroid Injections:
- Cortisone Injection should be considered in cases where mechanical interventions have failed.
- Cortisone injection should be considered in cases where there is an acute inflammatory process that has not been eased by mechanical therapies.
Acupuncture:
- Acupunture should be considered in cases where mechanical interventions have failed
- Acupunture should be considered in cases where there is an acute inflammatory process that has not been eased by mechanical therapies.
Extracorpeal Shock Wave Therapy:
- Extracorpeal Shock Wave Therapy should be considered in cases where mechanical interventions have failed and the patients have had symptoms for more than 6-months
Mechanical Plantar Fasciitis- 5th Line Intervention
Surgery:
- In cases that do not respond to any conservative treatment after 12 months, surgical evaluation can be considered for MPF